August 20 marks Southern HIV/AIDS Awareness Day (SHAAD)—a pivotal moment to spotlight the ongoing HIV crisis in the Southern United States and recommit to equity, visibility, and community-driven solutions.
A Region in Crisis: Disproportionate HIV Burden
The U.S. South, and especially the “Deep South” of Alabama, Florida, Georgia, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, and Texas, faces a uniquely severe HIV epidemic. In 2022, the region accounted for a staggering 52% of all new HIV diagnoses, despite composing only 38% of the U.S. population. At the same time, 14% of people living with HIV (PLWH) in the South were unaware of their status, highlighting critical gaps in testing outreach according to AIDSVu.
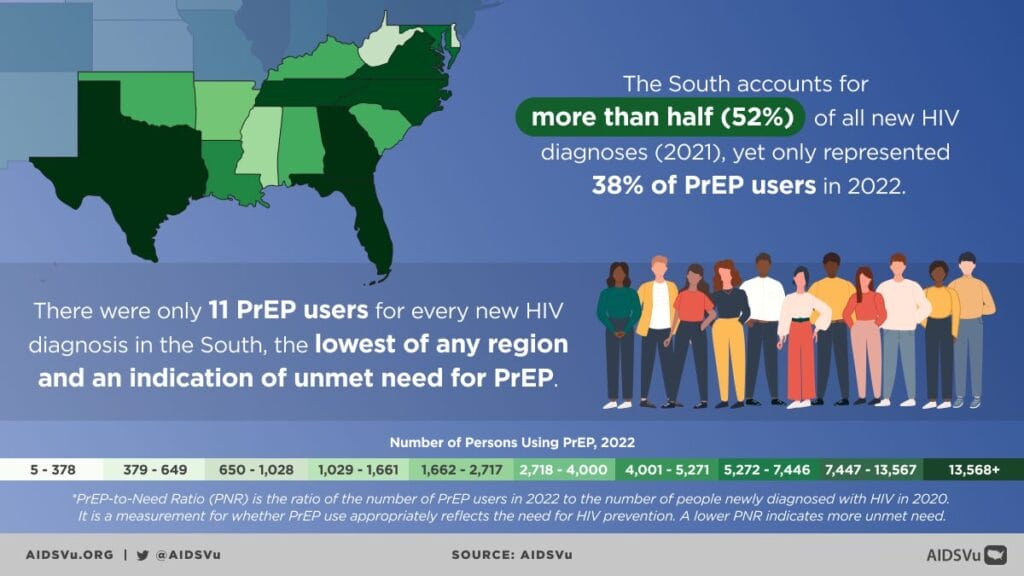
Prevention Gaps: The PrEP-to-Need Disparity
Prevention efforts fall short across the region. In 2024, the South recorded the country’s lowest PrEP-to-Need Ratio (PnR), with just 12 PrEP users for every new HIV diagnosis, signaling a vastly unmet need for HIV prevention services.
Inequities and Social Drivers Fuel the Epidemic
The South’s HIV crisis cannot be disentangled from the region’s entrenched social and structural inequities. High rates of poverty, low household income, housing insecurity, and systemic barriers create environments where prevention, testing, and treatment become out of reach.
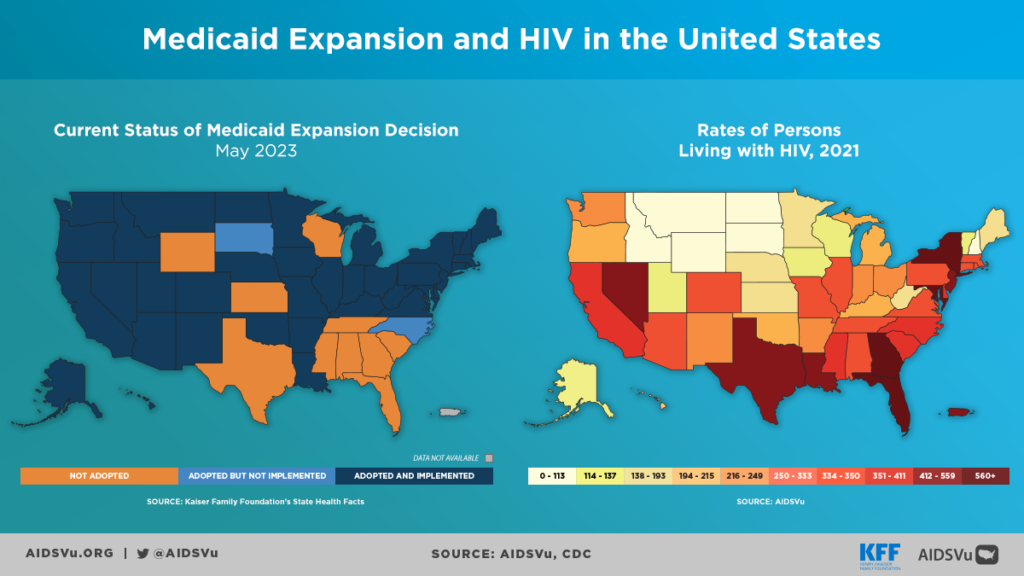
Healthcare access is particularly strained: nearly half of all uninsured Americans reside in the South. Medicaid expansion, a key lever for access, remains out of reach in nine of 17 Southern states as of 2023. Notably, states that expanded Medicaid have seen 1.4 times higher PrEP use than those that did not according to AIDSVu.
In rural areas, the situation is even more dire: limited transportation, long travel distances, provider shortages, and scarce culturally competent care deepen disparities, especially for those living far from urban centers.
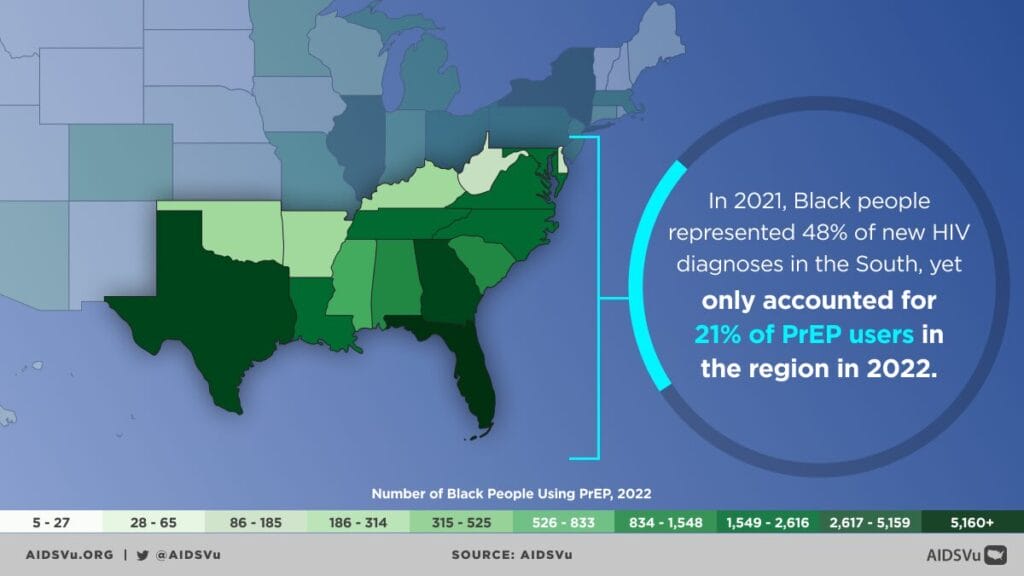
Communities of Color Disproportionately Affected
The HIV epidemic in the South is not evenly distributed, it falls hardest on Black and Hispanic communities, revealing long-standing inequities in health access, education, and prevention.
In 2022, Black individuals accounted for nearly 48% of all new HIV diagnoses in the South, despite making up less than one-fifth of the region’s population. Yet, by 2024, only 23% of PrEP users in the South were Black, highlighting a stark prevention gap (AIDSVu). This disparity underscores the reality that while Black communities are most impacted by HIV, they remain the least likely to benefit from lifesaving prevention tools.
The trend is similar for Hispanic communities. In 2022, Hispanic individuals made up 26% of new HIV diagnoses, but just 19% of PrEP users in 2024 (AIDSVu). These gaps reflect systemic barriers, from limited access to culturally competent healthcare to immigration-related fears that may deter people from seeking services. Language barriers, mistrust of healthcare systems, and stigma around sexuality and HIV further widen the gap.
These disparities don’t exist in a vacuum, they are shaped by social determinants of health such as poverty, housing instability, and limited health coverage. Nearly half of all Americans without health insurance live in the South, and the lack of Medicaid expansion in nine Southern states creates an uneven landscape of access. For many Black and Hispanic people, especially in rural areas, this means fewer clinics, longer travel distances, and higher out-of-pocket costs for care.
Stigma and Structural Barriers
Stigma also plays a particularly damaging role in communities of color. HIV stigma is often layered with racism, homophobia, and anti-immigrant sentiment, creating additional barriers to testing and treatment. For example, Black gay and bisexual men in the South face not only stigma related to their sexual identity but also systemic inequities in employment, healthcare, and criminal justice that exacerbate vulnerability to HIV. Similarly, many Hispanic individuals, particularly those who are undocumented, fear discrimination or legal consequences if they seek healthcare, limiting their access to testing and PrEP.
Yet, despite these challenges, communities of color in the South have long been at the forefront of advocacy. Black-led and Latinx-led community organizations continue to fill the gaps left by healthcare systems, offering free testing, PrEP navigation, peer support, and education tailored to the cultural realities of the people they serve. Supporting and investing in these grassroots organizations is critical to closing the gaps in HIV prevention and care.
Technological lag is yet another barrier. Many Southern states have been slow to adopt antigen/antibody combination HIV tests, which detect infection earlier when it’s most transmissible. Early diagnosis is vital to linking people to treatment and reducing onward transmission AIDSVu.
Rural communities face additional threats: the opioid crisis heightens risk for HIV and hepatitis C. As of 2016, nearly 68% of counties vulnerable to injection-related outbreaks were concentrated in the South AIDSVu.
Federal Efforts: Ending the HIV Epidemic Initiative
In response to persistent inequities and the urgent need for stronger solutions, the federal government launched the “Ending the HIV Epidemic: A Plan for America” (EHE) initiative in early 2019. The plan set an ambitious goal: to reduce new HIV infections in the United States by 90% by the year 2030. To achieve this, EHE focuses on four key strategies, diagnose, treat, prevent, and respond, that aim to close gaps across the HIV care continuum.
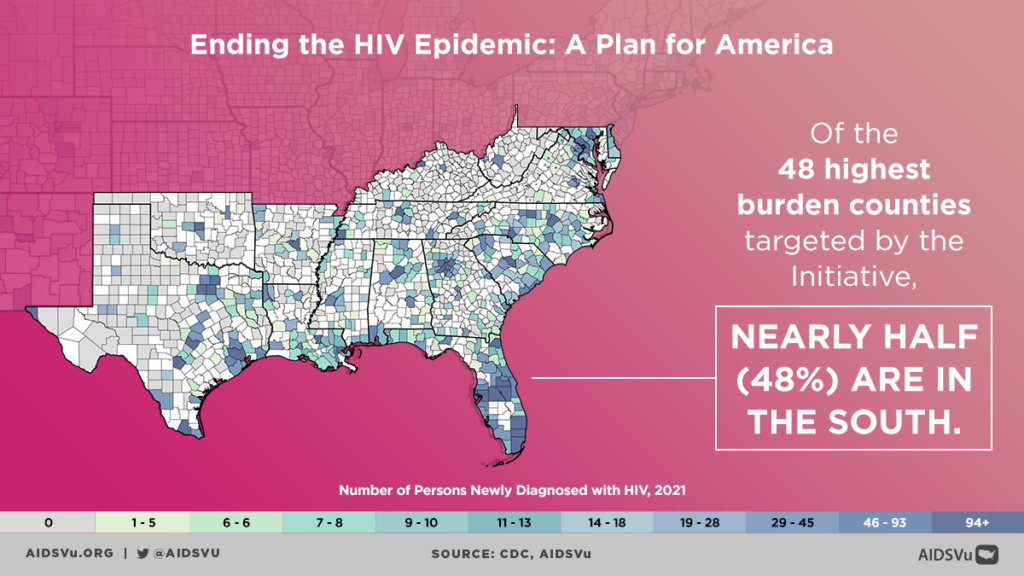
The initiative specifically targets 48 high-burden counties, along with San Juan, Puerto Rico; Washington, D.C.; and seven states with substantial rural HIV burden. Nearly half (48%) of these high-burden counties are located in the South (AIDSVu), underscoring how critical the region is to the nation’s overall HIV response.
However, despite its promise, the initiative was launched under the Trump administration, whose broader policies and actions undermined progress against HIV. While EHE funding was announced, the administration simultaneously rolled back protections for LGBTQ+ people and women in healthcare, restricted immigration policies that impacted access for immigrant communities, and appointed individuals with a history of opposing LGBTQ+ rights to key public health positions. These actions created mixed signals, slowed research momentum, and left many local organizations scrambling to fill resource gaps.
As a result, delayed funding rollouts, inconsistent leadership, and competing priorities meant that much of the South was left without the urgent scaling up of resources that EHE promised.
What makes the EHE plan especially vital for the South is its recognition of both urban and rural challenges. Metropolitan hubs like Atlanta, Miami, and Houston continue to rank among the highest for new HIV diagnoses, while rural communities in Alabama, Mississippi, and other Deep South states face longer travel times to clinics, shortages of HIV specialists, and persistent stigma. Yet, without fully resourced and consistent federal support, both urban and rural areas remain stuck in cycles of inequity.
The Biden administration has worked to restore momentum by reinvesting in public health infrastructure, supporting LGBTQ+ protections, and reaffirming the 2030 goal. Still, the damage of slowed progress during the Trump years is felt most acutely in the South, where communities already faced steep uphill battles.
A Call to Action This SHAAD
On August 20, Southern HIV/AIDS Awareness Day, we must confront this crisis head-on. AIDSVu’s 2025 SHAAD toolkit urges action to address health inequities and social determinants, and to expand prevention, testing, and care services in the South. So what can we do?
Amplify Community Voices
Elevate stories from those living with or affected by HIV in Southern LGBTQ+ communities.
Collaborate with grassroot initiatives in the South like the The Knights and Orchids Society, Southern AIDS Coalition, Women with a Vision, Nashville CARES, and more HIV focused groups based in the South
Advance Structural Change
Advocate for Medicaid expansion across all Southern states to widen healthcare access.
Invest in mobile clinics, telehealth platforms, and transportation solutions to reach rural and underserved areas.
Prioritize Equitable Prevention
Push for better PrEP access in Black and Hispanic communities via community-led outreach, culturally responsive messaging, and provider training.
Encourage adoption of early-detection technologies, like antigen/antibody HIV tests, to improve diagnosis rates.
Fight Stigma
Center stigma-reduction campaigns that resonate culturally and linguistically with Southern LGBTQ+ populations.
Train healthcare providers in affirming, inclusive care; challenge misinformation and bias.
Support Federal and Local Initiatives
Raise awareness of the EHE initiative and ensure that Southern jurisdictions are prioritized and equipped to scale HIV services effectively.
Mobilize resources for grassroots Southern organizations doing the day-to-day work of prevention, care, and advocacy.
Southern HIV/AIDS Awareness Day is more than a date serves as a reminder of the South’s ongoing HIV crisis, rooted in systemic inequities and reinforced by access barriers. But it is also a call to activate, to uplift, and to hold ourselves accountable to communities most impacted.
GLAAD, in solidarity with Southern advocates, can harness visibility, narrative power, and policy influence to change the trajectory of the epidemic. By centering social determinants, combating stigma, and expanding equitable access, we can move toward an empowered, HIV-free future for the South.