By: Courtney Johnson, Communities of Color and Media Consultant and MPV Subject Matter Expert
Even as monkeypox virus (mpox) transmission ebbs and begins to trend downward, it is still important to acknowledge that the unequitable vaccine rollout persists when it comes to reaching and serving communities of color.
Black people currently make up 34% of total mpox cases, accounting for more diagnoses than any other racial group. However, in addition to making up the majority of mpox cases, Black people are amongst the groups that have the lowest rates of vaccination against mpox. To discuss this disparity in vaccine rollout and total mpox cases within the Black community, as well as the ways that they have seen mpox disproportionately affecting Black communities and communities of color, I sat down with Dr. Leo Moore and Henry Philyaw.
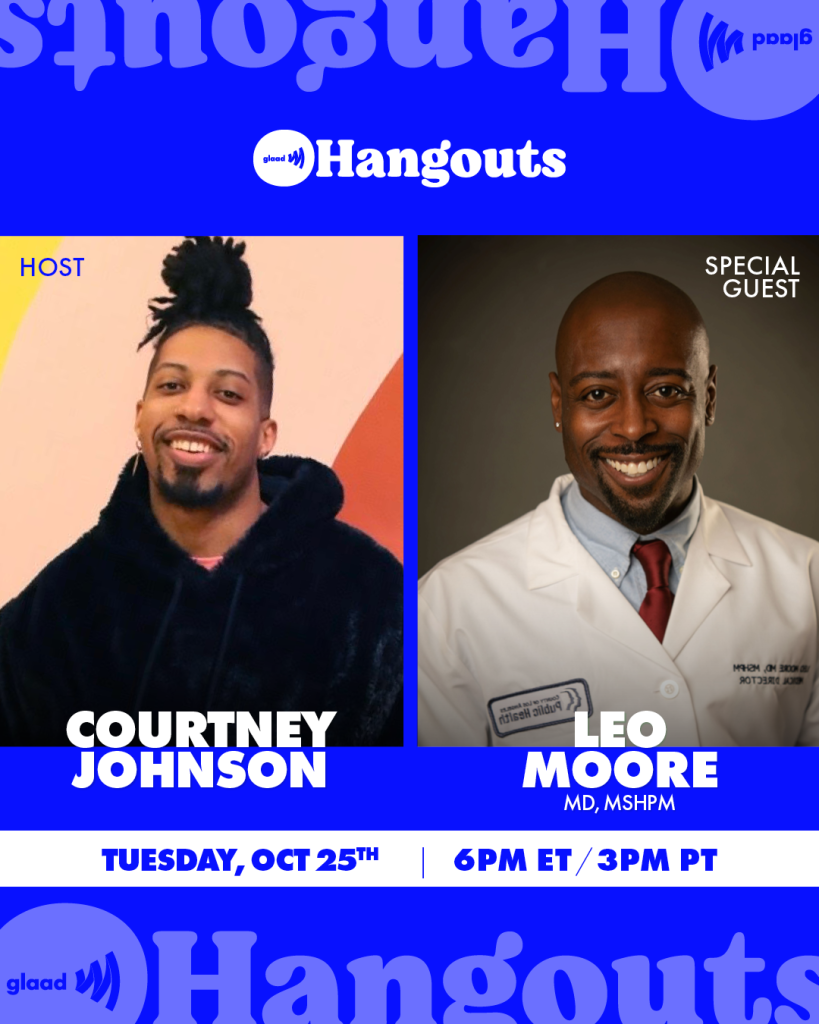
Joining me for an installment of GLAAD’s IG Live GLAAD Hangouts series, Dr. Moore, the Medical Director for Clinic Services at the Los Angeles Department of Health, discussed how, from the beginning, Los Angeles commited to an “equitable rollout” of the vaccine. While Los Angeles is among the top five cities in the United States with the most mpox cases since the onset of the health outbreak, California has recently experienced only a 1% monthly increase in total mpox cases.
Dr. Moore explained how Los Angeles prioritized certain populations, specifically those people who knowingly came into contact with mpox, and then expanded the criteria and sites as more vaccine became available and as more vulnerable communities emerged. California has had 5,547 mpox cases, and has administered over 256,858 doses of vaccine, with the number of vaccinated individuals continuously growing.

Comparatively, chiming in from the opposite coast, Henry Philyaw, a resident of Brooklyn, NY, described his experience trying to access the mpox vaccine as difficult. Henry was not able to schedule an appointment during the initial release of NYC vaccination appointments, and was only able to obtain his vaccination appointment by using his close personal network and connections. After finally scheduling an appointment, Henry arrived at his vaccination location in Harlem only to realize that the line of people waiting did not reflect the occupants and demographics of the neighborhood.
He vividly recalled that the majority of the staff administering the vaccine were Black, while the the majority of those receiving the vaccine were white. Many Black and Black Queer residents of the neighborhood were left without the opportunity to obtain the vaccine during it’s initial rollout in NYC. Recognizing this disparity and gap in care, Philyaw managed a kind of hotline where he used his own personal resources to help other queer people of color get vaccinated during the initial stages of the mpox outbreak.
“This was not like COVID, we could not miss work, there was no financial compensation,” says Philyaw, as we discussed the unique economic inequalities, obstacles, and threat that mpox poses to vulnerable, marginalized communities.
There’s a clear disconnect when Black people cannot access resources in their own communities, and are also the most impacted by mpox and the most vaccinated. Black people were not only outsourced in their own communities, bu there was no expansion of resources to give them access.

Most recently, mpox messaging has dwindled, and so have vaccination efforts towards the Black community. Black people initially received 13% of vaccinations, which would appear to be proporitionate to the population. However, when you consider the comparable response to the HIV epidemic and access to critical care, intervention, and prevention, it is clear that generic approaches do not work, and communities of color will suffer under them.

There must be a new blueprint for addressing health crisis that takes into consideration the unique experiences of Black queer people. As long as a one-size-fits-all approach continues to be utilized, healthcare and the healthcare system for communities of color will continue to be inadequate and inefficient.
To help the public maintain a downward trend in cases and transmission, people should continue to get vaccinated against mpox to protect their communities. Located at the end of our previous mpox community blog is a list of places to get vaccinated and where to locate services near you. If your city is not listed, be sure to contact your local health department for more information.