As monkeypox (MPV) cases continue to decline across the U.S., the social determinants of health, such as access to quality healthcare and housing, contribute to severe MPV in some gay and bisexual men and are causing public health officials to take a more holistic approach to treatment.
“MPV is not a virus that lives in isolation. It exists as a part of a number of acute and chronic outbreaks and health challenges that interact with each other and can be impacted by social circumstances that worsen disease outcomes,” writes Monkeypox National Response Deputy Coordinator Dr. Demetre Daskalakis along with other health officials for HIV.gov.
In one study published by the Centers for Disease Control and Prevention (CDC), nearly 40% of people diagnosed with MPV were also living with HIV, and over 40% had been diagnosed with a sexually transmitted infection (STI) in the year before their MPV diagnosis.
Dr. David Folkes, MD is the Community Health Outreach Manager at THRIVE SS, an Atlanta-based non-profit providing support for Black same-gender-loving men (SGL) living with HIV. He tells GLAAD that the MPV data illuminates that HIV is more prevalent than most care to admit.
“We were working on the front lines, and when we looked at the requests that were coming in [in Fulton County] for vaccination, we saw that approximately 50% of all the persons who identified as men who have sex with men were living with HIV,” Folkes says.
“When you look at the intersection of HIV and monkeypox, you see where a lot of the social determinants of health that predisposed persons to monkeypox were very similar to those that predisposed people to HIV,” he says. “So using that prevention strategy was also a pre-prevention strategy that worked for HIV as well.”
According to Folkes, the prevalence of dual diagnoses of MPV and HIV in Black, gay and bisexual men presented public health officials with two opportunities. One, provide MPV and HIV testing, and two, extend care for individuals living with HIV to become virally suppressed, resulting in better overall health outcomes, as well as making HIV untransmittable (Undetectable = Untransmittable, U=U).
By taking a more holistic approach to tackling the current MPV outbreak, officials are also examining other inequities’ impact on the healthcare system, including how housing instability contributes to health challenges. 23% of Black patients diagnosed with MPV also experience homelessness, according to the same study by the CDC.
“We forget that homelessness is an epidemic,” Folkes says. “People don’t necessarily tend to treat it as a disease because it’s a social issue. When you think of people who are sofa surfing because of homelessness, they’re sleeping on a different couch or a different bed every night. When you think about people who are sex workers, homelessness is another underlying condition that predisposes several people to monkeypox,” he says.
MPV and mental health
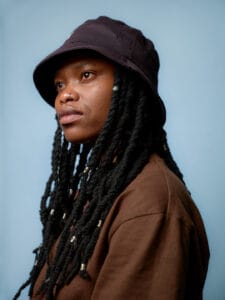
Harun Tulunay, 35, a gay man and sexual health worker diagnosed with HIV in 2016 and diagnosed with a severe case of MPV in June, fled government and familial persecution in his native Turkey. He settled in London in 2015.
Raised in a strict Islamic faith community, Tulunay tells GLAAD that relatives physically tortured him at age 18 for identifying as gay. He has completely severed ties with his parents, having last spoken to them over 15 years ago. As an immigrant to the UK, Tulunay says navigating his MPV diagnosis and quarantine alone without family support was daunting.
“It was very scary for me. I said I’m dying by myself at home. They will find my body at some point,” he says.
Tulunay was in quarantine for two weeks, preceded by a 104°F high-grade fever and a lesion covering most of his nose. He says his plea to local emergency services for medical intervention went ignored for nearly three weeks as his symptoms worsened. Despondent, physically ill, and without an official diagnosis, he decided to adhere to a self-imposed quarantine.
“Nobody told me to isolate [myself]. But I knew it was something infectious, so I thought, worst case, it’s COVID,” Tulunay says, having recovered from COVID-19 before.
“Can you imagine the mental state of just leaving somebody alone at home in isolation?”
Unlike his experience living with HIV, which in developed countries is now a chronic manageable condition, Tulunay says his anxiety about MPV and COVID increased in isolation.
“I didn’t struggle much [physically] with Covid, but I struggled [mentally] with the fear of it because people were dying,” he says. “But with monkeypox, I didn’t know anything about it, and many people still don’t. It’s been around since the 70s, but we didn’t look into it until it became a white man’s problem. We are still ignoring that people are dying in Africa,” he adds.
Classified as an endemic disease in West and Central Africa, the first case of human MPV was recorded in the Democratic Republic of Congo in 1970. After that, more than 400 MPV patients were documented in Africa between 1970 and 1990. The first outbreak outside Africa occurred in the United States in 2003 after human contact with pet prairie dogs.
Tulunay says the response from health and government officials in the U.K. and other developed countries worldwide has defined which groups of people have access to treatment and solutions during the current MPV outbreak—while leaving other groups out.
“You cannot just give it to white people and then completely ignore the rest of the communities all around the world while inequalities continue,” he says. “You cannot expect to end the virus while prioritizing wrongfully.”
Folkes agrees.
“If it’s not affecting persons of a particular experience or part of a particular socioeconomic status, it’s a disease that doesn’t matter,” he says.
But for many gay and bisexual men wearing the visible scars of MPV, a community-focused holistic approach centered around vaccine equity to protect vulnerable populations, matters. Folkes urges gay and bisexual men to remain vigilant as cases decline.
“Cases are going down, and people are getting less interested in vaccination. Fine, we get it. But when people stop vaccinating, we’re going to start seeing the numbers continue among those communities where people aren’t vaccinating,” he says. “And then we [must not] forget that monkeypox is not a gay disease. It’s something that affects everybody.”
To date, data suggests that gay, bisexual, and other men who have sex with men make up the majority of cases in the current MPV outbreak. However, anyone of any sexual orientation or gender identity is at risk if they are in close personal contact with someone who has MPV.
As Tulunay enjoys relief from his painfully isolating experience with MPV, he is ringing the alarm about the virus and other infectious disease threats facing gay and bisexual men. Despite being a target for anti-LGBTQ harassment online as an outspoken gay Asian man living with HIV, Tulunay is raising his voice across the U.K. and his native Turkey, often at risk of bodily harm. The remaining scar on his nose from the MPV lesion makes it nearly impossible for him to forget all he’s endured since the start of summer.
“It is a reminder of this condition, of being unable to access help and being in a hospital room for 11 days,” he says. All the unknowns—scary times.”
After fully recovering from MPV and undergoing seminal fluid testing, with no trace of the virus found in his body, Tulunay says he’s ready to get back to life as he once knew it. “I wasn’t able to have sex or date anyone, for a really long time,” he says. “I couldn’t go back to that mindset, but after the seminal testing, I got my mojo back.”