This report brings an academic and personal voice of the impact that the COVID-19 pandemic has had to-date on the fight to end the HIV epidemic, while also providing recommendations / needs from people at community-based organizations (CBOs) who serve and support the community. We underscore the disruption in access to HIV prevention and care services due to mitigation measures imposed in the early days of the COVID-19 pandemic, which will have implications for many years to come. We also highlight innovation to HIV service delivery that provided an important bridge between healthcare professionals and clients in an unprecedented time. Our recommendations will help sustain the fight against HIV in the United States in the midst of this pandemic, and future health emergencies.
PRE-PANDEMIC STATE OF HIV IN THE US
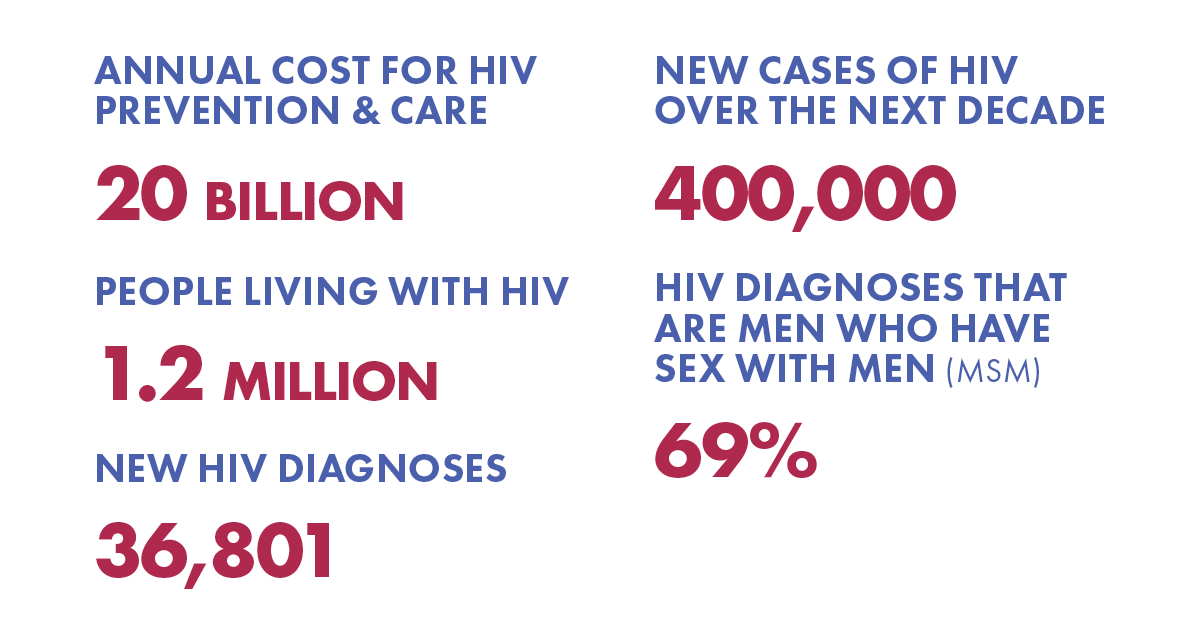
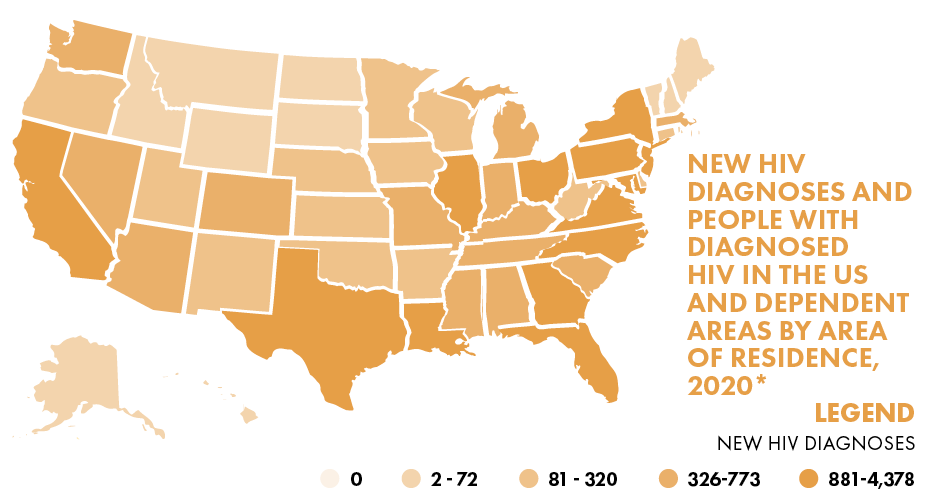
In 2019, 1.2 million people were living with HIV in the U.S. and there were 36,801 new HIV diagnoses.Given the new cases of HIV annually it is estimated that without intervention nearly 400,000 moreAmericans will be newly diagnosed over the next 10 years despite the availability of tools to preventtransmissions. Sexual minority men (SMM) including gay, bisexual, and other men who have sex withmen made up 69% of all new HIV diagnoses in 2019. The U.S. government spends $20 billion in annualdirect health expenditures for HIV prevention and care. There is a real risk of an HIV resurgence due toseveral factors, including trends in injection and other drug use; HIV-related stigma; homophobia andtransphobia; lack of access to HIV prevention, testing, and treatment; and a lack of awareness that HIVremains a significant public health threat.
PRE-PANDEMIC EHE HIV PREVENTION GOAL:
Ending the HIV Epidemic (EHE) Initiative focuses resources on areas where HIV transmission occursmost frequently, which funds communities to design and implement local programs to: Diagnose, Treat,Prevent, and Respond. The goal of the EHE is to reduce new HIV infections by 75% in five years and by90% in ten years.

DISPROPORTIONATE IMPACT OF COVID-19 IN THE U.S.

According to the CDC, racial minority communities in the U.S are 2-3 times more likely to be hospitalized and die due to COVID-19 complications compared to White, non-hispanic Americans.
CAUSES OF DISPROPORTIONATE IMPACT
- Structural Racism
- Underlying health comorbidities
- Living in high density neighborhoods
- Employment in public- facing occupations
- Societal inequities such as limited access to COVID testing
- Disparities in COVID vaccination rates
Effects of COVID on HIV
TESTING
- 68 – 97% reduction in HIV testing
- 17% decrease in HIV diagnosis
PREVENTION
- Surge of public information on COVID overshadowed other topics and health issues like prevention of HIV transmissions
- Client services were greatly reduced (or eliminated)
- 72% decrease in new PrEP initiation
CARE
- Detrimental impact on mental health
- Increased anxiety and depression
- Support services shuttered or not as utilized in a virtual environment
- Telemedicine – while an important bridge – wasn’t as optimal as in-person